Hemarthrosis And Its Causes
Hemarthrosis causes can be anything from trauma to the joint to neurological problems or even bleeding disorders. People who already suffer from a bleeding or blood clot disorder have a higher risk of experiencing hemarthrosis.
Heres a look at some of the reasons people suffer from joint bleeding:
Injury/trauma: A serious sprain or trauma to the extremities that impacts the major joints can lead to bleeding within that specific joint area.
Infection: Some infections can lead to articular bleeding
Haemophilia: Those who suffer from this hereditary condition, which impairs blood-clotting mechanisms, are more likely to get hemarthrosis.
Medications: Anticoagulants such as warfarin have the potential to lead to joint bleeds.
Clutton joint: This is inflammation of the joints in those who have been diagnosed with congenital syphilis.
Hemorrhagic Syndrome: There are people whose mucous membranes have a tendency to bleed and they are usually suffering from some type of hemorrhagic syndrome.
Knee joint arthroplasty: This is another way of saying a knee replacement.
Crimean-Congo hemorrhagic fever: This is a virus that is usually spread by tick bites or through contact with livestock that is carrying the disease.
Neurologic deficits: There are cases of neurological deficits that have been linked to hemarthrosis.
Osteoarthritis: Although rare, spontaneous hemarthrosis has been seen in elderly people who suffer from osteoarthritis.
How Do Orthopedic Surgeons Prevent Blood Clots After Procedures
Joint replacement surgeries, especially those of the lower extremities, are becoming increasingly more common today. One of the major risk factors associated with this type of surgery is a postoperative complication known as deep vein thrombosis .
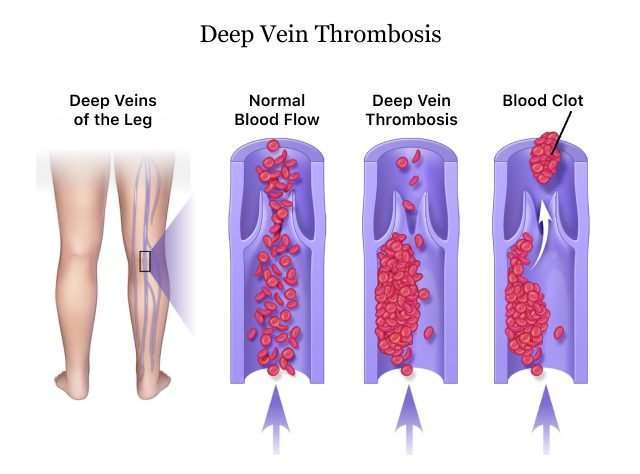
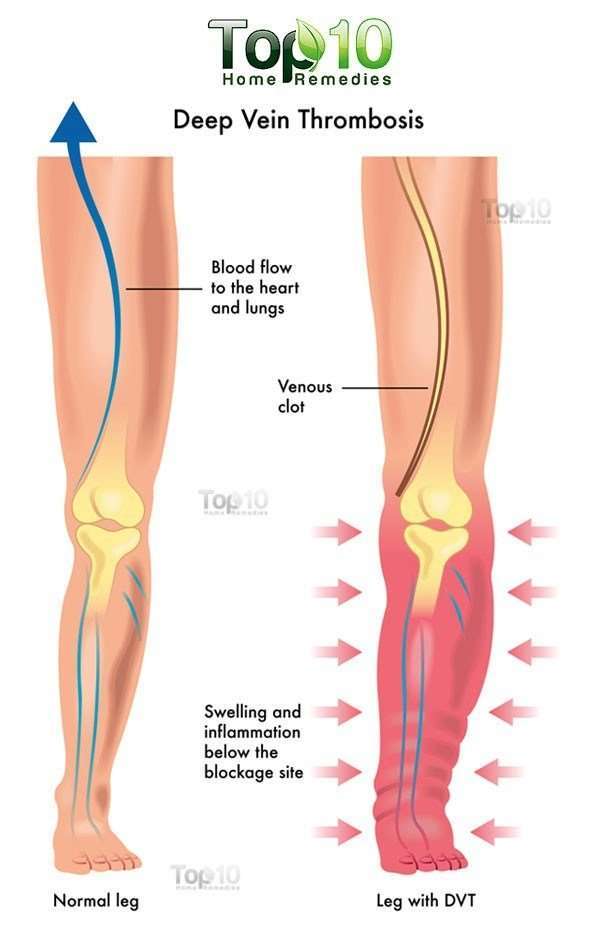
A DVT is the formation of a blood clot within a deep vein, and this typically occurs in either the calf or thigh. While DVT can develop after any kind of major surgery, patients who undergo lower extremity surgeries are particularly vulnerable.
Following hip surgery, thrombi often develop in the thigh veins. These clots are more likely to lead to pulmonary embolism than those that form deep within the calf following a knee procedure. While clots in the calf are less likely to lead to PE, they can be harder to detect.
Prevention of Blood Clots
Blood clot prevention is an approach used by Los Angeles orthopedic surgeons to specifically address coagulation and stasis issues. Generally, they utilize several therapies in combination. Patients will likely be fitted with elastic compression stockings, as well as an external compression device, when they are initially admitted to hospital.
Movement and rehabilitation exercises commence on the first postoperative day, typically continuing for several months following surgery. In addition, anticoagulant therapy usually begins the night before the surgical procedure, continuing for a prescribed period at home.
Early Movement and Rehabilitation
Mechanical Prevention
Drug Prevention
Aspirin
How Can Your Surgical Care Affect Your Risk For A Blood Clot
Certain aspects of your surgical care can also increase your risk for a blood clot. For example, blood clots are more likely the longer your surgery takes, and if you get spinal anesthesia versus general anesthesia or general anesthesia combined with an epidural. How long you remain immobile after your surgery can also affect your risk for a blood clot.
Recommended Reading: How To Use Ginger For Knee Pain
Symptoms Of Blood Clots In The Lungs After Surgery
It is important to know that many patients have no symptoms when they have a blood clot in the lungs. However, patient who have symptoms have a worse outcome than those without any symptoms. In the above mentioned Japanese study, patients who had symptoms had a mortality rate of 4.2% compared to all patients diagnosed with blood clots in the lungs after surgery.
Although you can have a blood clot in the lungs after surgery without any symptoms, it is important to pay attention to these symptoms because they indicate worse outcomes.
Here is the list of signs and symptoms:
Unfortunately, a sudden cardiac arrest is one of the symptoms of blood clots in the lungs after surgery. A cardiac arrest from a blood clot is very difficult to revive even when CPR and advanced life-saving measures are started right away.
Other Information About Preventing Blood Clots
- Some people who do not take medicine to prevent blood clots still have bleeding problems, although the risk for bleeding is lower.
- Warfarin takes at least several days to work.
- Your blood will need to be checked daily until your doctor makes sure you have the right amount of medicine. Once your medicine has been adjusted, your blood may be checked every 1 to 4 weeks.
- You may need to have someone come to your home to draw blood for this test or you may need to go to the doctors office or a lab to have blood drawn for this test.
Read Also: Arthritic Knee Remedies
Develop An Exercise Regime With Your Physical Therapist And Walk As Much As You Can Tolerate
This will help you heal and keep your blood flowing. It is very important to exercise, take your medicine as your doctor prescribes, or use the compression stockings during this time when you are healing. Enlist family and friends to help you with walks and exercisesâyou might need the additional motivation, and its best to walk with someone.
for an example of the exercises you will be doing with your physical therapist.
Why Choose The Tops
Anyone considering back surgery should also be aware that some procedures for treating a spinal problem may present lower risks or provide better outcomes than others. For example, the TOPS procedure, which may be performed after spinal decompression surgery to stabilize the spine, provides better clinical outcomes than spinal fusion surgery, which was the traditional choice for spine stabilization before the introduction of the TOPS system.
The TOPS provides for minimally invasive spine surgery and thereby significantly reduces the risks associated with DVT. Previously, when knowledge in spine treatment wasnt as developed as today, the fusion procedure was the only available and most innovative option. The vertebrae were glued into a relatively rigid structure, which significantly limited movement. Even though flexion and extension werent possible, and the risks were very impressive, the fusion continues to be performed today. However, TOPS surgery has become a more acceptable alternative to treating degenerative spondylolisthesis of lumbar spinal stenosis for many younger physicians. Its advantage is movement in all axial directions, as well as stability.
The structure is implanted using a traditional posterior surgical approach, but the TOPS system exerts less force on the screws than other configurations.
You May Like: What Causes Your Knee To Lock Up
Important Safety Information & Indications
For people taking ELIQUIS for atrial fibrillation: Do not stop taking ELIQUIS without talking to the doctor who prescribed it for you. Stopping ELIQUIS increases your risk of having a stroke.
ELIQUIS may need to be stopped prior to surgery or a medical or dental procedure. Your doctor will when you should stop taking ELIQUIS and when you may start taking it again. If you have to stop taking ELIQUIS, your doctor may prescribe another medicine to help prevent a blood clot from forming.
ELIQUIS can cause bleeding, which can be serious, and rarely may lead to death. This is because ELIQUIS is a blood thinner medicine that reduces blood clotting.
You may have a higher risk of bleeding if you take ELIQUIS and take other medicines that increase your risk of bleeding, such as aspirin, nonsteroidal anti-inflammatory drugs , warfarin, heparin, selective serotonin reuptake inhibitors or serotonin norepinephrine reuptake inhibitors , and other medicines to help prevent or treat blood clots. Tell your doctor about all of the medicines you take, including any over-the-counter medicines, vitamins, and herbal supplements.
While taking ELIQUIS, you may bruise more easily and it may take longer than usual for any bleeding to stop.
-
headaches, or feeling dizzy or weak
ELIQUIS is not for patients with artificial heart valves.
ELIQUIS is not for use in people with antiphospholipid syndrome , especially with positive triple antibody testing, who have a history of blood clots.
Prevention And Treatment Of Blood Clots After Hip And Knee Replacement Surgery
Taking steps for the prevention and treatment of blood clots after hip and knee replacement surgery is an important part of your recovery. Joint replacement patients are at highest risk for developing a DVT two to 10 days after surgery, and remain at risk for approximately three months.To prevent the occurrence of a blood clot, your doctor will likely prescribe a combination of treatment approaches for you, which may include:
- Exercise/physical therapy beginning the first day after surgery and continuing for several months
- Compression stockings
- Anti-clotting medicine to reduce the bodyâs ability to form blood clots
Recommended Reading: What Is The Best Knee Walker
Will Your Bones Even Allow For A Revision Knee Replacement
An August 2019 study in the Journal of Orthopaedic Surgery and Research offered this warning to surgeons concerning the problems of identifying whether a patients bones were strong and dense enough to withstand another knee replacement procedure.
Revision total knee arthroplasty is a demanding procedure, with a high complication and failure rate and a high rate of bone losses and poor bone quality. Different classifications for bone losses have been proposed, but they do not consider bone quality, which may affect implant fixation.
Look at the study findings:
- Fifty-one patients were included .
- The most frequent cause of failure was:
- aseptic loosening of the implant .
- 18.9% of the cases demonstrated poor bone quality.
What the researchers of this study were seeking to point out is that if revision knee replacement is required, a plan to address and repair the possibility of bone loss, bone weakening, a loss of bone density should be undertaken. This would significantly increase the success of the replacement.
Preventing Blood Clot Formation
As you can probably surmise based on the above paragraphs, the best way to prevent blood clots is to stay active after surgery. We know this wont always be easy, but even just standing and moving for a couple minutes can really help push blood through your body. Aside from safe physical activity, other ways to prevent blood clot formation after hip or knee replacement include:
- Staying hydrated
- Working to get to an ideal weight before and after surgery
- Giving up smoking
- Wearing compression stockings
- Knowing the signs and symptoms of a blood clot
The last point is key, because time is of the essence when it comes to treating a potential blood clot. Some symptoms to be on the lookout for include pain or tenderness in your legs, unexpected swelling, shortness of breath, leg discoloration and chest pain. If you are experiencing any of these symptoms, contact your surgeon or another healthcare provider right away.
We work hard to minimize your risk of blood clot formation by performing joint replacement techniques that avoid damaging blood vessels when possible, even though the maneuver is more complex for the surgeon. Dr. Botero has extensive experience performing these more complex procedures because he knows its worth it to provide a higher level of patient safety. To learn more about his hip or knee replacement techniques and how he can help reduce your risk of a blood clot after your joint replacement operation, reach out to his clinic today at 558-4444.
Don’t Miss: Why Does My Knee Hurt When It’s Cold
Help What Do These Weird Symptoms Mean
As you recover from your ACL surgery, you fully expect a tender, achy knee but a painful lower leg or difficulty breathing?those are completely unexpected. If after the first few days post-surgery you notice an increase in pain, or a new pain located in your calf or chest, it is time to drop everything and contact your surgeonIMMEDIATELY. You may have a life-threatening blood clot.
A most sobering topic, blood clots develop when a vein becomes obstructed or constricted. The blood, with no place to go, backs up, pools, coagulates and a clot is born. And then the danger begins: DVTs can wreak havoc on delicate surrounding tissue and possibly kill you when a portion of the clot breaks off and travels from the leg to the chest, lodging in an artery in your lungs. This is known as a Pulmonary Embolism or PE, and its ghastly.
Make it one of your top goals to reducethe possibility of a DVT in every way you can. Strive for optimal wellness before and after surgery: quit smoking, manage your weight, stay active, and let your surgeon know if you are on oral contraceptives , and then wear your compression stockings, take your aspirin, and keep moving. Flow freely with these following tips.
Medical Devices To Prevent Dvts And Pes
|
|
|
|
|
|
|
|
|
| Comparing medicines and medical devices |
|
|
| Comparing specific medical devices |
|
|
| Taking medicine for 28 days or longer |
|
|
Don’t Miss: What Is Chondrocalcinosis Of The Knee
What Can Cause Knee Pain Years After A Knee Replacement
Knee replacements dont last forever. Most knee replacements perform well and cause no issues to patients for 10 to 20 years after the operation. When pain occurs years after knee replacement, its typically due to one of these four knee replacement problems after 10 years or more.
- Soft tissue irritation around the knee The most common pain patients experience that occurs years after a knee replacement will be the soft tissue around the knee. Patients still have multiple tendons, ligaments, and muscles around the knee that may become irritated with varying activities.
- The implant becomes loose A loosening implant is a cause of pain that can occur years after knee replacement surgery. A loosening implant is typically caused by wear and tear over time, though it can be exacerbated by high-impact sports or obesity. A loosening implant can cause pain as well as instability in the knee and a change in the alignment of the knee joint.
- Infection The infection rate after knee surgery is very low, around 1 percent. If an infection does set in around the components of the knee replacement, it can be difficult to treat with antibiotics. Revision surgery may be necessary to get the infection under control.
Read Also: How To Whiten Knees And Elbows
Clotting Complications: Deep Vein Thrombosis And Pulmonary Embolism
Deep Vein Thrombosis is a blood clot, commonly found in the leg or thigh, that can form as a result of stagnant blood flow, coagulation, and damage to vein walls.
According to Dr. Anne Bass, chairperson of the Deep Venous Thrombosis Prevention Committee at HSS, DVTs can cause leg pain and swelling. Clots can also travel to the lung, causing a pulmonary embolism, which is a blockage of arteries that traverse the lung.
When left untreated, DVTs can inflict damage on the vein where the clot is located, causing chronic swelling and even ulceration,” she explains. “Pulmonary emboli can produce symptoms of shortness of breath, chest pains, a rapid heart rate, or fainting. In very rare cases, a fatal blockage of pulmonary arteries may occur.
Also Check: Inversion Table After Hip Replacement
Discussing How To Prevent Blood Clots With Your Doctor
You and your doctor will need to discuss which medicines or devices might be best to prevent blood clots after hip or knee replacement surgery or surgery for a broken hip. Medicines can help prevent blood clots, but they can also slightly increase your risk for bleeding. For most people, the risk of getting a blood clot after surgery is higher than the risk of bleeding while taking the medicine. The treatment your doctor suggests may depend on several factors, including:
- The options available at the hospital.
- Your medical history and other medical conditions you have.
- Your particular risks.
______________________________________________________________________