Risk Factors For Knee Arthritis
- Age. Osteoarthritis is a degenerative, wear and tear condition. The older you are, the more likely you are to have worn-down knee joint cartilage.
- Heredity. Slight joint defects or double-jointedness and genetic defects may contribute to osteoarthritis in the knee.
- Excess weight. Being overweight or obese puts additional stress on the knees over time.
- Injury. Severe injury or repeated injury to the knee can lead to osteoarthritis years later.
- Overuse. Jobs and sports that require physically repetitive motions that place stress on the knee can increase risk for developing osteoarthritis.
- Gender. Postmenopausal women are more likely to have osteoarthritis than men.
- Autoimmune triggers. While the cause of rheumatoid arthritis remains unknown, triggers of autoimmune diseases are still an area of active investigation.
- Developmental abnormalities. Deformities such as knock knee and bowleg place higher than normal stress on certain parts of the knee joint and can wear away cartilage in those areas.
- Other health conditions. People with diabetes, high cholesterol, hemochromatosis and vitamin D deficiency are more likely to have osteoarthritis.
How Is Ra Diagnosed
RA is diagnosed by reviewing symptoms, conducting a physical examination, and doing X-rays and lab tests. Its best to diagnose RA earlywithin 6 months of the onset of symptomsso that people with the disease can begin treatment to slow or stop disease progression . Diagnosis and effective treatments, particularly treatment to suppress or control inflammation, can help reduce the damaging effects of RA.
Whats The Big Difference With Osteoarthritis
Osteoarthritis happens through wear and tear, which is why its more common in people aged 50+. By contrast, RA is a disorder of the immune system, where the body starts to attack its own tissues. This leads to inflammation, which can stretch the knee capsule and degrade the lining cartilage. In some cases, osteoarthritis follows from that.
Read Also: What To Do If Your Knee Hurts When You Walk
Do I Need A Knee Replacement
If you have severe knee pain and continued destruction of the knee that isnât getting better with RA medications, and you already have damage to your knee joint, your doctor may recommend a total knee replacement. This surgery is very successful for severe RA. More than 80% of patients are happy with the surgery and resume most normal activities for up to 15 years.
Though knee replacement works for many people, rates of knee replacements among RA patients have declined over the years. This is probably because new and better treatments, like biologics, for RA help people avoid surgery.
During a knee replacement, your doctor removes the damaged cartilage and bone and replaces it with a plastic or metal joint. The surgery itself takes a couple of hours and usually requires general anesthesia. Youâll stay in the hospital for 1-3 days.
About one in 25 people with RA develop an infection after a total knee replacement. This is a slightly higher infection rate than for people who get a knee replacement for another reason, like osteoarthritis. A few reasons why this may be include:
- A weaker immune system
- More muscle weakness
How Is Knee Arthritis Diagnosed
Your doctor may use some of the following diagnostic tests and procedures to determine if you have knee arthritis:
- Medical history and physical examination
- Blood tests for genetic markers or RA antibodies
- X-rays to determine cartilage loss in the knee
- Joint aspiration: drawing out and testing the synovial fluid inside the knee joint
Cartilage cannot be seen on X-ray, but narrowing of the joint space between the bones indicates lost cartilage. X-rays show bone spurs and cysts, which can be caused by osteoarthritis. Other tests such as MRI or CT scans are rarely needed for diagnosis.
Recommended Reading: Why Does My Knee Swell
Rheumatoid Arthritis In The Hands
One of RAs first noticeable features can be seen in the hands. Swelling of the knuckle joints and wrists leads to severe pain and stiffness, especially in the morning.
Chronic inflammation can cause the fingers to twist in an outward direction. This can take a toll on fine motor skills. In advanced cases of RA, the hands can permanently change shape and interfere with your quality of life.
With proper treatment, you can manage your RA symptoms. Treatments focus on reducing the inflammation in order to prevent joint damage.
For hands and fingers, these treatments may include oral medications and splinting. Splinting helps support the joints, but splints shouldnt be worn for too long because this may lead to muscle deterioration.
Certain injections may help too. A doctor may recommend a combination of steroids to reduce inflammation and anesthetics to help ease associated pain.
The effects of steroid injections can last for several months, but a doctor may exercise caution in repeating these treatments because of possible side effects. Side effects include:
of people with RA report symptoms in the feet and ankles. This includes damage to the ligaments as well as other issues with the toes.
These symptoms can lead to pain and mobility difficulties.
Different Types Of Arthritis Very Different Treatments
The goal of treatment for both is to improve movement, reduce pain, and minimize joint damage, but the way to that is different for each disease, says Dr. Rackoff. Here’s what to expect:
RA The first line of defense is using disease-modifying anti-rheumatic drugs to reverse chronic inflammation. Anti-inflammatories, pain meds, and physical therapy are also used. It may take some time to determine which medication works optimally for your specific circumstances. A person may even need to try a few different types of medicine or a combination of medications. No two people, even with the same diagnoses, are alike in how they respond to various treatments. Its a puzzle that has to be put together by you and your doctor, says Dr. Wilmarth. Its very important to keep an open and honest dialogue with your doctor and healthcare team in general and especially in order to ideally reach and maintain remission with RA.
The goal with RA and other autoimmune illnesses is to treat to target . This sets remission or low disease activity as a goal. Patients are monitored frequently with their rheumatologist and adjustments to their treatment protocol are made as necessary.
RELATED: Your Rheumatoid Arthritis Plan: When Remission Is the Target
Read Also: What Type Of Dr For Knee Pain
What Are The Symptoms Of Rheumatoid Arthritis
The joints most often affected by RA are in the hands, wrists, feet, ankles, knees, shoulders, and elbows. The disease often causes inflammation in the same areas on both sides of the body. Symptoms may begin suddenly or slowly over time. Each persons symptoms may vary, and may include:
These symptoms can seem like other health conditions. Always see your healthcare provider for a diagnosis.
Steroid Injections Worsen Knee Arthritis According To Two New Studies
by Radiological Society of North America
Two studies comparing injections commonly used to relieve the pain of knee osteoarthritis found that corticosteroid injections were associated with the progression of the disease. Results of both studies were presented today at the annual meeting of the Radiological Society of North America .
Osteoarthritis is the most common form of arthritis, affecting 32.5 million adults in the U.S. Knee osteoarthritis is a chronic, degenerative and progressive condition with an estimated incidence of 800,000 patients each year. More than 10% of patients with knee osteoarthritis seek noninvasive treatment for pain relief through corticosteroid or hyaluronic acid injections.
Researchers in both studies chose cohorts from the Osteoarthritis Initiative, a multicenter, longitudinal, observational study of nearly 5,000 participants with knee osteoarthritis currently in its 14th year of follow-up.
In the first study, researchers at the University of California, San Francisco included 210 Osteoarthritis Initiative participants, 70 of whom received intraarticular injections, and a control group of 140 who did not receive injections during a two-year period. Of the 70 patients who received injections, 44 were injected with corticosteroids, and 26 were injected with hyaluronic acid. The treatment and control groups were matched by age, sex, body mass index, pain and physical activity scores, and severity of disease.
You May Like: Why Is My Knee Hurting When I Walk
Pseudogout: Calcium Pyrophosphate Deposition
Pseudogout is a type of inflammatory arthritis that results from the buildup of calcium pyrophosphate crystals in the joints of the body. While less common than gout, pseudogout is more likely to affect the knee.
Like gout, pseudogout is caused by a build-up of microscopic crystals in a joint and can lead to sudden, severe knee pain, swelling, warmth, and redness. Pseudogout is less common than gout but more likely to affect the knee joint.
The microscopic crystals that cause pseudogout are called calcium pyrophosphate crystals. Doctors often refer to pseudogout as calcium pyrophosphate deposition .
Pdus: Synovitis By Pdus
was performed in each scanning plane as described above. In addition the infrapatellar longitudinal scan was scored for hypervascularisation. The semiquantitative findings of PDUS activity for synovitis were scored as follows: Grade 0 = no intraarticular colour signal, grade 1 = up to 3 single colour signals or 2 single colour signals and 1 confluent colour signal representing only low flow, grade 2 = greater than grade 1 to < 50% of the intraarticular area filled with colour signals representing clear flow, grade 3 = > 50% of the intraarticular area filled with colour signals .
A sum score for the knee was applied according to a recently published scoring system for large joints , including the sum of the synovitis scores in the GSUS and the PDUS modes. The range for the sum score for the knee was 0-12 in GSUS and 0-15 in PDUS.
Don’t Miss: Which Doctor Do I See For Knee Pain
Rheumatoid Arthritis Vs Osteoarthritis
The pain and progression in each of the diseases are different. They can seem to be somewhat similar in that they both cause pain and decreased function. But then their similarities diverge, says , doctor of physical therapy, a health and patient advocate and CEO of Back2back Wellness and a psoriatic arthritis and osteoarthritis patient.
Look for these differences:
Rheumatoid Arthritis In The Knee: Symptoms And Treatments

| | | |
More than 1.3 million people in the U.S. have rheumatoid arthritis , which typically starts in the hands and fingers and can later progress to the knees. The resulting joint stiffness, pain, and swelling affecting the knees can restrict movement, potentially impacting quality of life.
To learn more about knee RA, myRAteam spoke with rheumatologist Dr. Iris Navarro-Millán, assistant professor of medicine at Weill Cornell Medicine and the Hospital for Special Surgery in New York City, and a National Institutes of Health -funded rheumatology researcher specializing in knee RA.
Because knee RA shares some symptoms with knee osteoarthritis , another form of arthritis, making a diagnosis can be challenging, Dr. Navarro-Millán said. When people with RA start experiencing knee pain, we tend to jump quickly to say, You probably also have osteoarthritis. But it’s very common for with RA to have both.
Many members of myRAteam report late-stage knee pain. Ive had RA for 10 years, but only experienced pain in my knees in the last one or two years, explained one member.
Getting a correct diagnosis, however, has been frustrating for some. My doctor said I dont have RA because its in my knees, yet everything I’ve read said that RA can attack the knees, one member said. Another member added, My rheumatologist was way too quick to assume my knee pain was fibromyalgia and OA, not RA. Im getting a second opinion.
You May Like: How Do I Know If Knee Pain Is Serious
Laboratory And Clinical Parameters
The mean ESR was 34.9 mm/h ± 25.1 while the median DAS 28 was 4.60 . The DAS28 revealed a significant higher disease activity in the group which received systemic GCs than in the group receiving only intraarticular GCs at baseline , while significant values were reached between these groups comparing T3 to T0. The exact values for each group are listed in .
Rheumatoid Arthritis And The Eyes
In some cases, inflammation from RA can make the whites of your eyes red and swollen, which may indicate a condition called scleritis. Scleritis can cause symptoms such as pain, light sensitivity, and blurry vision.
Uveitis is another eye condition associated with RA. It causes inflammation between the whites of your eyes and the retina.
Both scleritis and uveitis can lead to permanent eye damage if left untreated.
RA may also increase your risk of dry eye and glaucoma.
Its also possible to develop Sjögrens disease, an autoimmune condition that causes inflammation in the tear-producing glands of the eyes. Artificial tears may help treat dry eye associated with Sjögrens.
Recommended Reading: What Causes Arthritis Pain In The Knee
How Is Rheumatoid Arthritis Diagnosed
Diagnosing RA may be difficult in the early stages. This is because symptoms may be very mild, and signs of the disease may not be seen on X-rays or in blood tests. Your healthcare provider will take your medical history and give you a physical exam. Tests may also be done, such as:
- X-ray. This test uses a small amount of radiation to create images of internal tissues, bones, and organs onto film.
- Joint aspiration. For this test, a small fluid sample is taken from a swollen joint. It is done to look for signs of infection or gout.
- Nodule biopsy. Tiny tissue samples are taken to look at under a microscope. This helps to check for cancer or other abnormal cells.
- Blood tests. These tests are done to find certain antibodies, called rheumatoid factor, cyclic citrullinated antibody, and other signs of RA.
- Ultrasound or MRI. These imaging tests can look for bone damage and inflammation.
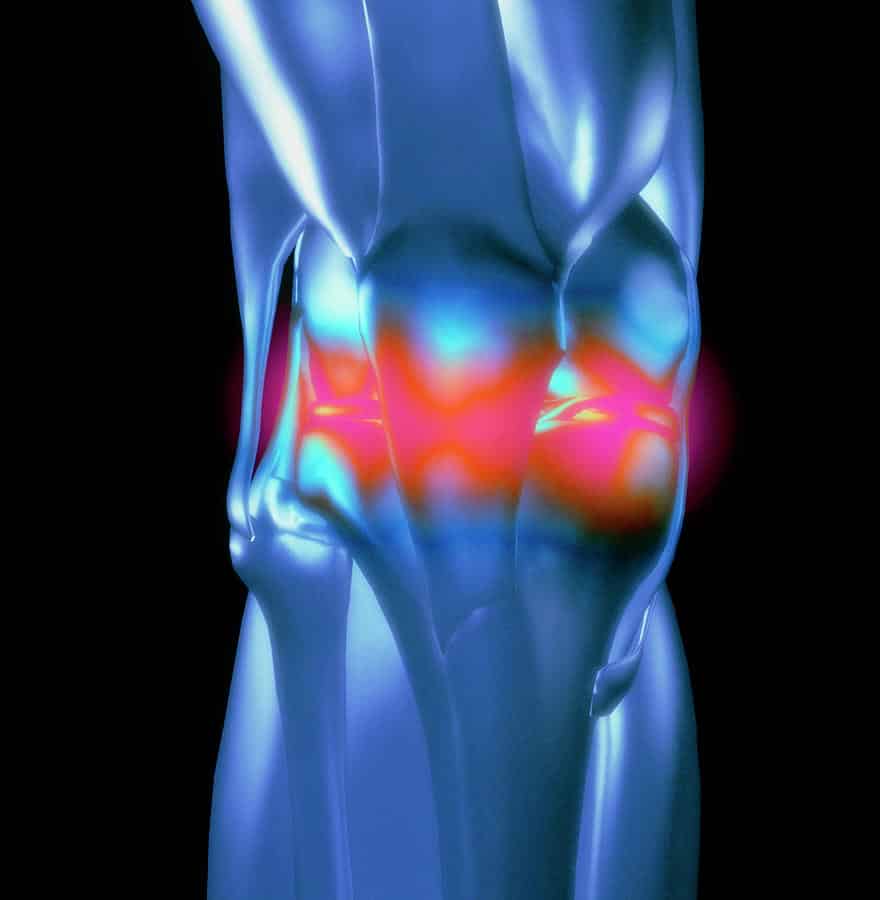
Where Can Arthritis Occur In The Knee
Cartilage loss can occur between the thighbone and the shinbone in the medial portion , lateral portion and under the kneecap.
- Thinning of the cartilage under the kneecap is called patellofemoral arthritis .
- Some patients have cartilage loss in one, two or all of these areas. When all three areas are affected, this is called tricompartmental arthritis.
Read Also: Black Lace Up Knee High Boots
Difference Between Osteoarthritis And Rheumatoid Arthritis
There are several different types of arthritis. Osteoarthritis and rheumatoid arthritis are two of the most common forms. Although the symptoms of these two types of arthritis can be similar, it’s very important to distinguish between them in order to determine the proper treatment.
At the University of Michigan Health System, our experienced rheumatologists will do appropriate tests to determine which type of arthritis you have. Then we will develop an effective treatment plan and will explain your options.
Osteoarthritis occurs when the smooth cartilage joint surface wears out. Osteoarthritis usually begins in an isolated joint.
Rheumatoid arthritis is an autoimmune disease, which means that the immune system malfunctions and attacks the body instead of intruders. In this case, it attacks the synovial membrane that encases and protects the joints. Rheumatoid arthritis often targets several joints at one time. The symptoms of rheumatoid arthritis include:
- the symmetrical nature of the disease ,
The Location Of The Joint Pain
RA Most commonly these joints are affected: hands, wrists, fingers, elbows, knees, feet, and hips. However, the pain can be in any joint. The pain is usually symmetrical it effects both sides of the body at the same time.
OA There is pain wherever a joint has been injured or worn through overuse most commonly in the hands, fingers, thumb, knees, hips, lower back and neck. The pain is not symmetrical. The lifetime risk of developing OA of the knee is about 46 percent, and the lifetime risk of developing OA of the hip is 25 percent, according to the American College of Rheumatology.
Also Check: How Far Should I Be Walking After Knee Replacement
What Are The Signs And Symptoms Of Arthritis Of The Knee
There are many signs and symptoms of arthritis of the knee:
- Creaking, clicking, grinding or snapping noises .
- Difficulty walking.
- Joint pain that changes depending on the weather.
- Joint stiffness.
- Knee joint pain that progresses slowly or pain that happens suddenly.
- Your knee locks or sticks when its trying to move.
Pain and swelling are the most common symptoms of arthritis of the knee. Some treatments might reduce the severity of your symptoms or even stall the progression. See your healthcare provider if you have symptoms of knee arthritis.
How Does A Normal Joint Work
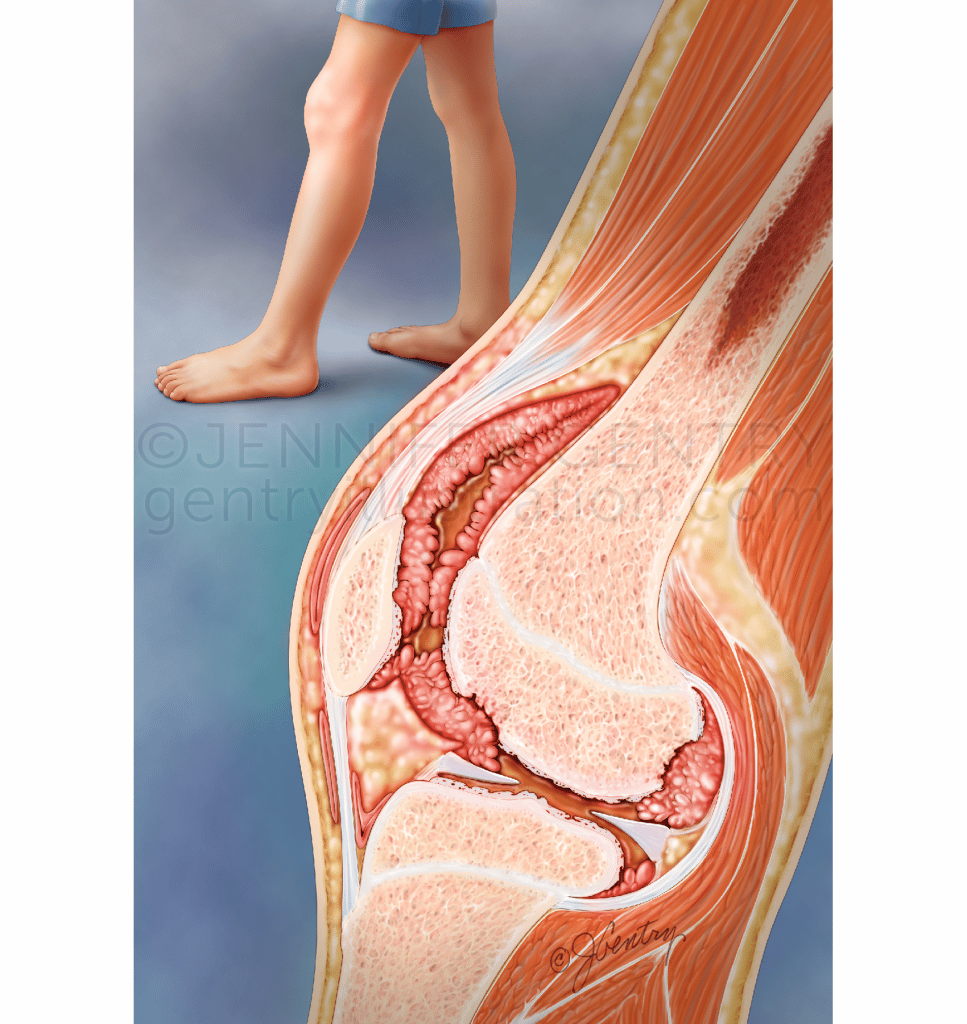
A joint is where two bones meet. Most of our joints are designed to allow the bones to move in certain directions and within certain limits.
For example, the knee is the largest joint in the body and one of the most complicated. It must be strong enough to take our weight and must lock into position, so we can stand upright.
It also has to act as a hinge, so we can walk, and needs to twist and turn when we run or play sports.
The end of each bone is covered with cartilage that has a very smooth, slippery surface. The cartilage allows the ends of the bones to move against each other, almost without rubbing.
The joint is held in place by the synovium, which contains thick fluid to protect the bones and joint.
The synovium has a tough outer layer that holds the joint in place and stops the bones moving too far.
Strong cords called tendons anchor the muscles to the bones.
Also Check: What Is Removed In Knee Replacement Surgery
Talk With Others Who Understand
On myRAteam, youll meet other people living with rheumatoid arthritis. More than 142,000 myRAteam members come together to ask questions, give advice, and share their stories with others who understand life with RA.
Have you been diagnosed with RA of the knee? Have you found effective ways to treat this condition? Share your experience in the comments below, or start a conversation by posting on your Activities page.