What Is Bilateral Knee Osteoarthritis
Bilateral Knee Osteoarthritis is a degenerative joint disease affecting both the knees as a result of the everyday wear and tear and gradual loss of articular cartilage.
The common symptoms associated with this type of Osteoarthritis include:
- Pain in both the knees which worsens with activity
- Stiffening of both the knees
- Swelling of both the Knees
- Pain in both the knees after prolonged sitting
Diseases Of The Musculoskeletal System And Connective Tissuenote
- certain conditions originating in the perinatal period
- certain infectious and parasitic diseases
- compartment syndrome
- complications of pregnancy, childbirth and the puerperium
- congenital malformations, deformations, and chromosomal abnormalities
- endocrine, nutritional and metabolic diseases
- injury, poisoning and certain other consequences of external causes
- symptoms, signs and abnormal clinical and laboratory findings, not elsewhere classified
- Osteoarthritis of bilateral knee patellofemoral joints
- Osteoarthritis of bilateral knees
- Osteoarthritis of bilateral patellofemoral joints
- Osteoarthritis of both knees
- Primary osteoarthritis of bilat knees
- Primary osteoarthritis of both knees
-
- 20162017201820192020202120222023Billable/Specific Code
Applicable To
What Is Osteoarthritis Of The Knee
Osteoarthritis of the knee happens when the cartilage in your knee joint breaks down, enabling the bones to rub together. The friction makes your knees hurt, become stiff and sometimes swell. While osteoarthritis in the knee cant be cured, there are many treatments to slow its progress and ease your symptoms. Surgery is an option for more severe forms of osteoarthritis.
Also Check: How To Walk Normal After Knee Surgery
What Role Did Versus Arthritis Play
ACI was originally developed by scientists in Goteborg. A group from The Robert Jones and Agnes Hunt Orthopaedic Hospital at Oswestry , led by the late Professor James Richardson, travelled to learn about this procedure and on their return began developing ACI treatment in the UK.
We funded research conducted at the Tissue Engineering and Regenerative Therapies Centre Versus Arthritis, led by Professor Sally Roberts, to understand the benefits that ACI can offer. This research showed that there are a number of factors such as a persons age, gender and number of previous surgeries that can affect how successful ACI is. That gives doctors valuable insight into deciding which people should be offered this procedure.
Evidence from these studies has been pivotal to the approval of the ACI procedure by the National Institute for Health and Care Excellence for use in people with small areas of cartilage damage or early osteoarthritis.
Professor Sally Roberts, who leads this research and featured on BBC Ones The One Show talking about ACI said: This treatment can make a difference in delaying the onset of osteoarthritis, particularly in younger people who have small areas of cartilage damage. While the procedure isnt suitable for everyone, it shows the positive impact of early intervention and the importance of understanding the condition at all its stages.
Is Surgery Used To Treat Knee Osteoarthritis
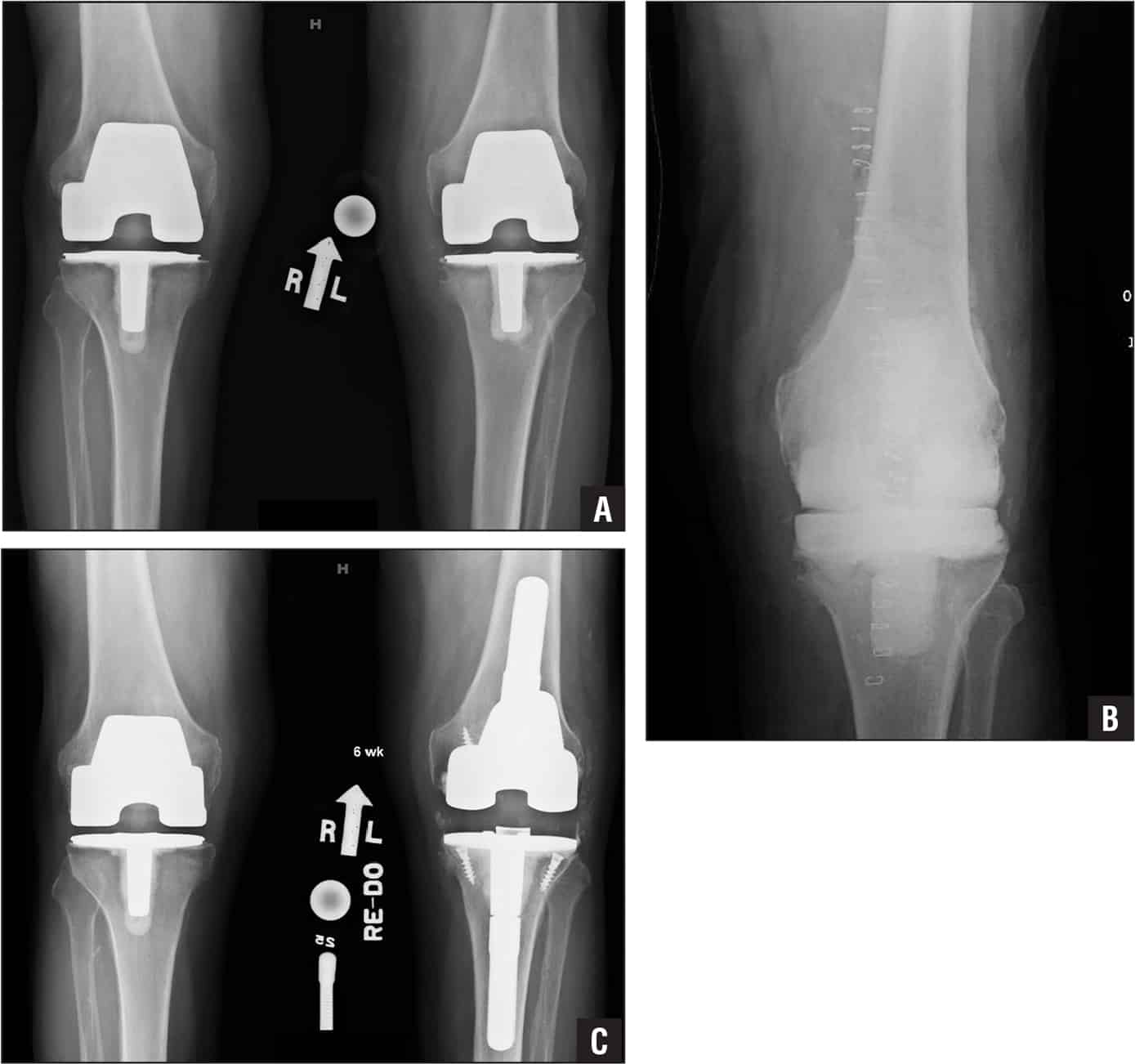
If your doctor wants to treat the osteoarthritis in the knee with surgery, the options are arthroscopy, osteotomy, and arthroplasty.
- Arthroscopy uses a small telescope and other small instruments. The surgery is performed through small incisions. The surgeon uses the arthroscope to see into the joint space. Once there, the surgeon can remove damaged cartilage or loose particles, clean the bone surface, and repair other types of tissue if those damages are discovered. The procedure is often used on younger patients in order to delay more serious surgery.
- An osteotomy is a procedure that aims to make the knee alignment better by changing the shape of the bones. This type of surgery may be recommended if you have damage primarily in one area of the knee. It might also be recommended if you have broken your knee and it has not healed well. An osteotomy is not permanent, and further surgery may be necessary later on.
- Joint replacement surgery, or arthroplasty, is a surgical procedure in which joints are replaced with artificial parts made from metals or plastic. The replacement could involve one side of the knee or the entire knee. Joint replacement surgery is usually reserved for people over age 50 with severe osteoarthritis. The surgery may need to be repeated later if the prosthetic joint wears out after several years. But with today’s modern advancements, most new joints will last over 20 years. The surgery has risks, but the results are generally very good.
Recommended Reading: Why Is My Knee Tight
How Can I Get Access To This Treatment
ACI is now available on the NHS. This means that more peopleacross the UK can access ACI and its benefits. However, it is only offered to specific patients, usually those with small areas of cartilage damage or early osteoarthritis, as set out by NICE guidelines. You can speak to your GP or consultant to find out more.
How To Diagnose Bilateral Knee Oa
The process has the same steps as unilateral knee osteoarthritis.
First, your doctor will ask about your joint pain and medical history. This is to look out for typical symptoms of this condition and identify any risk factors.
Next comes the physical exam. Here, your healthcare provider will inspect your knee and do a series of movement tests.
Read Also: Leg Numb From Knee Down
Pain Mechanisms In Osteoarthritis
Pain, the main presenting symptom of osteoarthritis, is presumed to arise from a combination of mechanisms, including the following:
- Osteophytic periosteal elevation
- Vascular congestion of subchondral bone, leading to increased intraosseous pressure
- Synovitis with activation of synovial membrane nociceptors
- Fatigue in muscles that cross the joint
- Overall joint contracture
- Joint effusion and stretching of the joint capsule
- Central pain sensitization
When the spine is involved in osteoarthritis, especially the lumbar spine, the associated changes are very commonly seen from L3 through L5. Symptoms include pain, stiffness, and occasional radicular pain from spinal stenosis. Foraminal narrowing is caused by facet arthritic changes that result in compression of the nerve roots. Acquired spondylolisthesis is a common complication of arthritis of the lumbar spine.
Having A Congenital Deformity
Certain deformities can make people prone to develop osteoarthritis. This is the case for people born with a valgus or varus deformity in the knees.
This anatomic malalignment will inevitably change the way your knee joint distributes the weight. So, one side will be under more stress than the other, making it prone to unilateral wear and tear.
Read Also: Pain On The Left Side Of The Knee
What Is Primary Osteoarthritis Of Knee
Primary osteoarthritis is caused by the breakdown of cartilage, a rubbery material that eases the friction in your joints. It can happen in any joint but usually affects your fingers, thumbs, spine, hips, knees, or big toes. Osteoarthritis is more common in older people.
Is knee osteoarthritis serious?
Knee arthritis can make it hard to do many everyday activities, such as walking or climbing stairs. It is a major cause of lost work time and a serious disability for many people. The most common types of arthritis are osteoarthritis and rheumatoid arthritis, but there are more than 100 different forms.
How Osteoarthritis Develops
Cartilage is a firm, but flexible tissue that covers the ends of the bones in your body. When two bones meet at a joint, the cartilage tissue helps absorb the forces that are transmitted through the area and reduce the amount of friction that occurs.
Osteoarthritis is the process by which inflammation or injury causes the bodys cartilage to wear down or thin in a particular joint. This degeneration, which usually occurs gradually over time, can alter the way your joint moves and increase the rubbing or friction in the area. In addition, the body responds to increased friction by building up excess bone in the joint which can further impede or alter your movement.
Read Also: How To Tape Your Knee
What Causes Osteoarthritis
Primary osteoarthritis is a heterogeneous disease meaning it has many different causes, it is not only âwear and tearâ arthritis. Some contributing factors to OA are modifiable and others are non-modifiable . Age is a contributing factor, although not all older adults develop osteoarthritis and for those who do, not all develop associated pain. As discussed above, there can also be inflammatory and metabolic risks that can increase the incidence of osteoarthritis, particularly in the setting of diabetes and/or elevated cholesterol.
Osteoarthritis can be genetic both as primary such as nodular OA of the hands as well as secondary related to other genetic disorders, such as hypermobility of joints. Inflammatory and infectious arthritis can contribute to the development of secondary osteoarthritis due to chronic inflammation and joint destruction. Previous injuries or traumas including sports-related and repetitive motions can also contribute to osteoarthritis.
Although the exact mechanisms of cartilage loss and bone changes are unknown, advancements have been made in recent years. It is suspected that complex signaling processes, during joint inflammation and defective repair mechanisms in response to injury, gradually wear down cartilage within the joints. Other changes cause the joint to lose mobility and function, resulting in joint pain with activity.
Tools For Optimized Coding

Automated ICD-10 coding and billing success improves office morale and increases staff retention.
Net Health Therapy for Clinics EHR is the solution that makes ICD-10 coding and other billing/compliance tasks simpler through automation and by providing the billing team access to a fully customizable, configurable coding and compliance engine.
Front-end, back-end, billers, and coders are thrilled with the job scheduling, accounting, and automated optimal coding. It is all the outpatient therapy EMR and billing software you need in one package to maximize ICD-10 coding, improve reimbursement, increase patient engagement and provide outstanding staff with excellent tools.
Don’t Miss: How Long Should You Ice Your Knee
Icd 10 Codes For Knee Pain
Yes, we are now going to map this ICD 9 code, 719.46 for knee pain in ICD 10. Here, I will show how the code in ICD 10 gives more information about the anatomic location. As I said the there are three ICD 10 codes for knee pain which will differ only in their 6th digit. As I have already shared about coding unilateral & bilateral diagnosis in ICD 10, here also same rule follows. Below are the three ICD 10 codes for knee pain ICD 9 code.
Knee pain ICD 10 codes
M25.561 Pain in right knee
M25.562 Pain in left knee
M25.569 Pain in unspecified knee
Now, as you can see above the sixth digit is only different in all the ICD 10 codes. Here, you can conclude that sixth digit 1 is for right side, 2 is for left side and 9 for unspecified side. This follows for all locations, which are present on both sides of the body. Hope, now you would have understood the difference between ICD 9 code and ICD 10 codes for knee pain.
Read also: How to clear CPC Exam in First Attempt
How Do I Know If I Have Osteoarthritis
Unlike other types of arthritis, the pain from osteoarthritis usually develops gradually over many months or years. Often it increases with activities that put stress on the joint, such as running or prolonged walking. Pain and joint swelling tend to increase slowly over time. Sometimes, especially in more advanced disease, a sensation of crunching or grinding may be noticed in affected joints. Prolonged morning stiffness is not a prominent symptom in OA as compared to inflammatory arthritides, such as rheumatoid or psoriatic arthritis. Osteoarthritis does not usually cause fevers, weight loss, or very hot and red joints. These features suggest some other condition or type of arthritis.
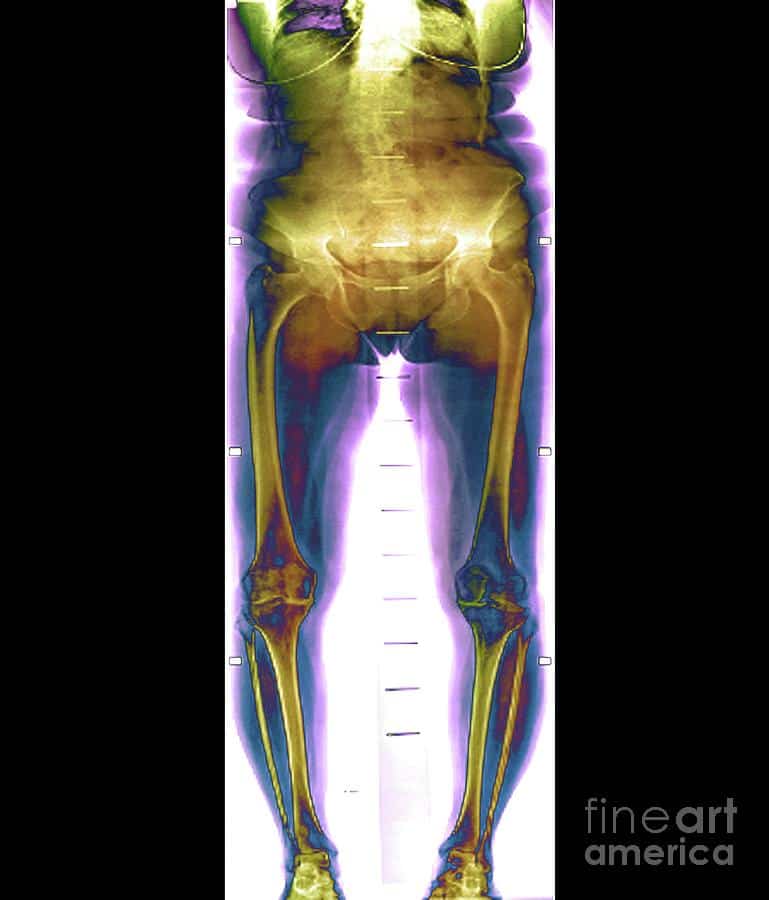
Your healthcare provider can typically diagnose osteoarthritis by obtaining a complete history of your symptoms and examining your joints. X-rays may be helpful to make sure there is no other reason for the pain. Magnetic resonance imaging is generally not needed except in unusual circumstances or in cases when the cartilage or surrounding ligament tear is suspected. There are no blood tests that diagnose osteoarthritis. If a joint is particularly swollen, a doctor may need to drain fluid from that joint. Tests can be performed on the fluid to look for clues for other types of arthritis, such as gout.
Don’t Miss: Why Do My Knees Hurt In The Morning
Mild Osteoarthritis Of The Knees
Unlike minor Osteoarthritis, those suffering from Mild Osteoarthritis may start to notice changes in their knee joints. Moreover, the radiographic images will also start to show certain changes in the joint due to the visible appearance of the osteophytes and thinning of the cartilage. Even though the bones’ space will still appear normal on the x-rays, the meeting point of the bones with the tissues will start to show visible hardening. This hardening can be seen by the thicker amount of bone present in this region with a denser appearance. These changes will lead to the individual experiencing some stiffness of the joint and pain on movement, which may worsen when the person is sitting for long periods of time.
What Is Autologous Chondrocyte Implantation
Autologous Chondrocyte Implantation involves the removal of a small sample of tissue from an individuals joints. This tissue is then used to grow a fresh supply of cartilage cells in a laboratory. Around three weeks later, these cells are returned to the damaged area of the joint in another operation, where they form new cartilage.
This procedure usually involves a short hospital stay of a day or two, followed by rehabilitation and physiotherapy as an out-patient. Someone who undergoes ACI can expect to resume full everyday use of the joint within three months and can start being more active around one year after treatment.
ACI has been shown to improve the symptoms of osteoarthritis, including pain and mobility. It can also slow or stop osteoarthritis developing, delaying or preventing the need for joint replacement surgery. This makes it particularly useful for younger people with early-stage osteoarthritis.
Read Also: Can Arch Supports Help Knee Pain
What Causes Osteoarthritis Of The Knee
Osteoarthritis of the knee happens when your knee joint cartilage wears out or is damaged. Articular cartilage is tough, rubbery tissue on the ends of your bones that lets you bend and move. Meniscal cartilage absorbs shock from pressure on your knee.
Your cartilage is like your cars shock absorber, protecting your car from bumps and jolts. Drive on lots of rough roads, your shocks wear out fast. Drive on easy streets, your shocks last longer. You can wear out or damage your knee joint cartilage if:
- Youre overweight. If your body mass index is 30 or more, youre seven times more likely to develop osteoarthritis in your knee than someone with a lower BMI.
- You injure your knee or have an old knee injury.
- You frequently put stress on your knee at your job or playing sports.
- You inherited a tendency to develop osteoarthritis of the knee.
- You have crooked bones or joints, such as having knocked knees.
What Is Osteoarthritis
Osteoarthritis, commonly known as wear-and-tear arthritis, is a condition in which the natural cushioning between joints — cartilage — wears away. When this happens, the bones of the joints rub more closely against one another with less of the shock-absorbing benefits of cartilage. The rubbing results in pain, swelling, stiffness, decreased ability to move and, sometimes, the formation of bone spurs.
Read Also: Do High Knees Burn Belly Fat
What Have We Achieved
Research funded by Versus Arthritis led to the development of a new treatment to repair damaged cartilage in early-stage osteoarthritis called Autologous Chondrocyte Implantation , which is now available on the NHS.
Marianne, who was treated with ACI, said The difference this treatment has made to me is incredible. I cant imagine where I would be without it. It has changed my life and I feel like I am back in control again.
Articles On Knee Osteoarthritis
While age is a major risk factor for osteoarthritis of the knee, young people can get it, too. For some individuals, it may be hereditary. For others, osteoarthritis of the knee can result from injury or infection or even from being overweight. Here are answers to your questions about knee osteoarthritis, including how it’s treated and what you can do at home to ease the pain.
Recommended Reading: Can Ms Cause Knee Pain
How Is Osteoarthritis Of The Knee Diagnosed
The diagnosis of knee osteoarthritis will begin with a physical exam by your doctor. Your doctor will also take your medical history and note any symptoms. Make sure to note what makes the pain worse or better to help your doctor determine if osteoarthritis, or something else, may be causing your pain. Also find out if anyone else in your family has arthritis. Your doctor may order additional testing, including:
- X-rays, which can show bone and cartilage damage as well as the presence of bone spurs
- magnetic resonance imaging scans
MRI scans may be ordered when X-rays do not give a clear reason for joint pain or when the X-rays suggest that other types of joint tissue could be damaged. Doctors may use blood tests to rule out other conditions that could be causing the pain, such as rheumatoid arthritis, a different type of arthritis caused by a disorder in the immune system.